A hospital admission refers to the time that a patient occupies a hospital bed under the care of hospital staff. More than 36.2 million people in the United States were admitted to the hospital in 2019, according to the most recent statistics from Statista. Additionally, the majority of those admitted consisted of seniors 65 years of age or older.
A hospital admission refers to the time that a patient occupies a hospital bed under the care of hospital staff. More than 36.2 million people in the United States were admitted to the hospital in 2019, according to the most recent statistics from Statista. Additionally, the majority of those admitted consisted of seniors 65 years of age or older.
Because hospital beds and staff are finite resources, the number of hospital admissions has a direct correlation to a hospital’s ability to coordinate consistent care to patients at varying levels of need. Hospital resources that are spread too thin can lead to a degradation in the quality of care. One of the best ways to avoid that is through patient education and by being proactive rather than reactive, when possible, during health care challenges.
Patients need to understand the key concepts of hospital admissions. Knowing what to expect, what to bring to the hospital and their rights removes many of the unknowns that can make being admitted to a health care facility intimidating or scary for patients. Keeping that in mind, the following details the key concepts, conditions and types of hospital admissions:
How Can Patients Get Admitted to the Hospital?
How patients are admitted to the hospital depends on individual circumstances and the critical nature of the injury or illness. For example, a patient who’s incurred severe head trauma in a car wreck and who’s unresponsive will be admitted differently from a patient who’s fractured a wrist falling off a bicycle.
Different health care scenarios lead to different methods of patient assessment and types of hospital admissions. However, some parts of the process are consistent across the board, such as the information collected during the patient registration process.
Registration for Admission
Except in the case of emergency admissions when the patient is unable to provide information, all patients must go through a registration process before being admitted to the hospital. This process enables hospital staff to collect a patient’s medical history and personal information to better coordinate care. The following are the pieces of information that patients will need to provide:
- Personal identifying information, such as full name and address
- Personal and emergency contact information, such as phone number and email address
- Health insurance information (carrier name, member number, group number)
- Signed authorization to release medical information to insurance company
- Signed hospital service agreement, includes consent to receive health care services and agreement to pay charges
Types of Hospital Admissions
Personal circumstances and the severity of the injury or illness are determinants in how a patient is admitted to the hospital. Below are the four main types of hospital admissions.
Planned Admission
A planned admission (aka elective hospital admissions) occurs when a patient has a health care condition that requires advanced treatment and hospitalization, which their primary health care provider or specialist is already aware of. In this case, patients work with their health care providers to conveniently schedule hospital admissions. The patients are usually given an estimate of how long they’ll be in the hospital based on the treatment or procedure that they’ll be receiving.
The major advantage of planned admissions is that physicians are better able to coordinate care for their patients and arrange beds and essential tests, such as X-rays and lab tests, prior to admission. This type of advanced planning and preparation can result in more favorable patient outcomes.
Emergency Admission
An emergency admission occurs when a patient has a life-threatening injury or illness that requires immediate medical attention. Common examples are heart attack, stroke and extreme trauma or blood loss. Patients in life-threatening situations are admitted to the hospital’s emergency department: a specialized unit within the hospital. Patients who are in stable condition are transferred from the emergency department to another department for observation and further treatment.
Direct Admission
A direct admission (aka direct admission hospitalization) occurs when a physician deems it necessary for a patient to be immediately admitted to the hospital. Typically, this occurs during an office appointment when a physician notices critical symptoms or receives test results that confirm a critical health care scenario.
A direct admission is viewed as a higher priority than a planned admission, but not as critical as an emergency admission. A direct admission patient is advised to go to the hospital as soon as possible, but is usually not in a life-or-death situation. Ultimately, the physician determines whether a patient can make it to the hospital on their own or needs an ambulance. Physicians who request that a patient be directly admitted usually make bed arrangements.
Transfer Admission
A transfer admission is any scenario in which a patient is transferred from a hospital bed to another floor, department or hospital. The physician who’s treating the patient often initiates the transfer. For example, an emergency admission patient who’s reached stable condition would be transferred from the emergency department to a different department for observation.
However, patients, their spouses or their caretakers can also request a transfer. This is usually brought on by determining that the patient would receive better care elsewhere.
For example, someone suffering from a stroke would be admitted to the closest emergency department in the area to receive immediate treatment. If neurosurgery were required, the family could request to have the patient transferred to another hospital with more experienced neurosurgeons on staff.
Regarding specialized surgeries involving the brain, heart or spine, it’s not uncommon for patient advocates to request transfers so that patients can be seen by the top professionals in their field of specialty. Additionally, a transfer admission occurs when a patient is brought to a hospital, but the hospital lacks the beds or the resources to provide adequate care.
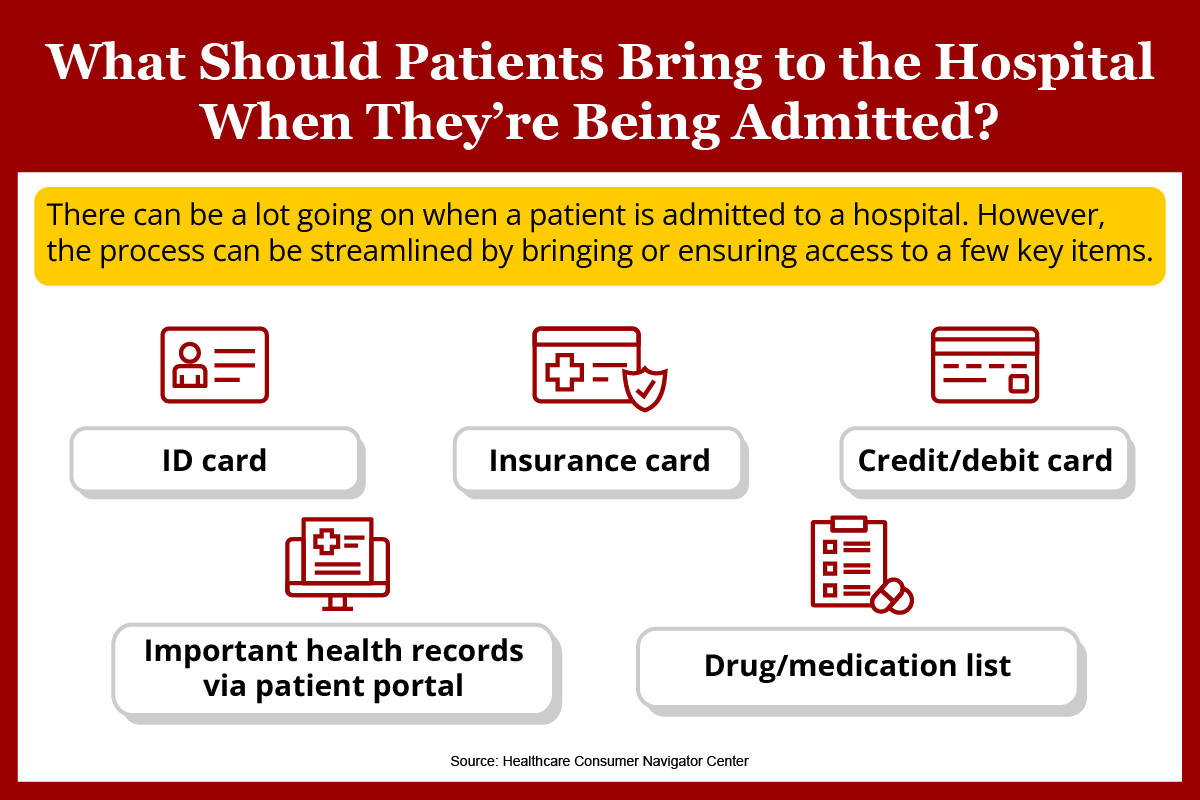
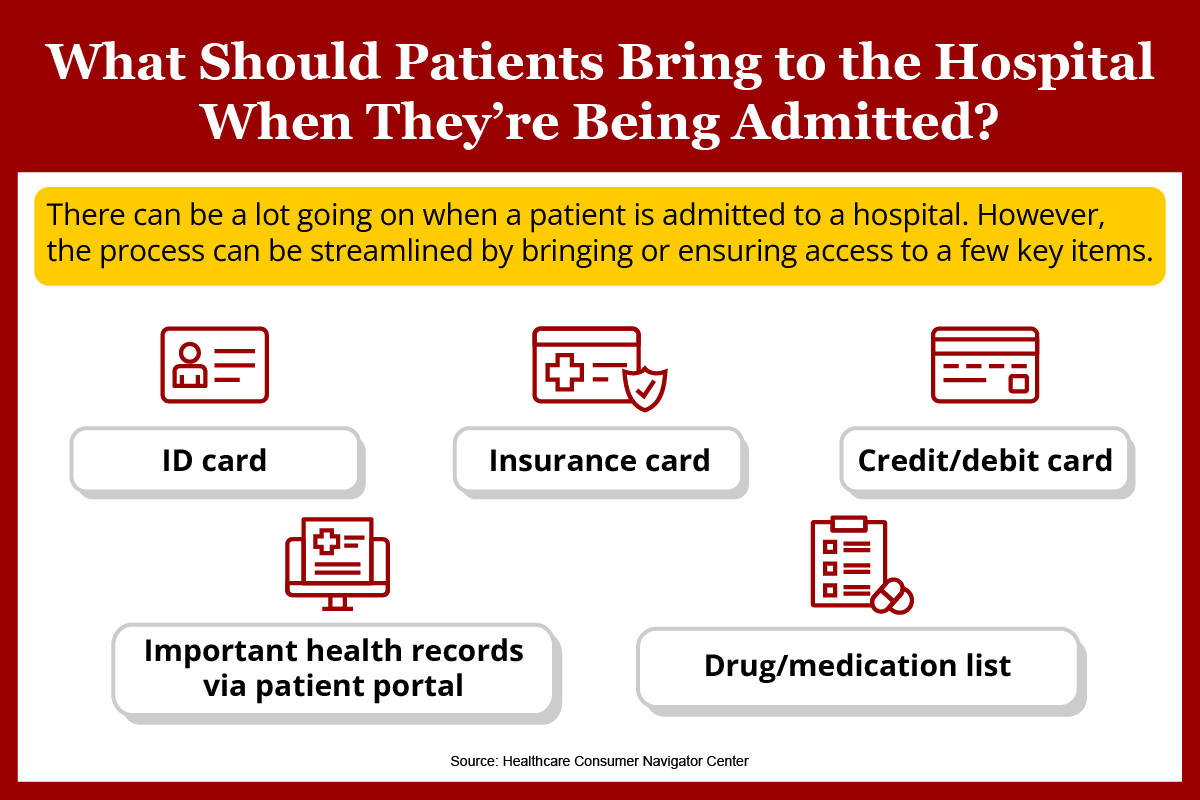
What to Bring to the Hospital
Patients who are due to be admitted to the hospital often wonder what documents and other items they should bring. What to bring to the hospital can be divided into two main categories: critical items and personal items.
Critical items include medical documents and other essentials that health care staff will need to treat the patients. This includes specific instructions from their physicians (most applicable in direct admits) and a full list of medications, drugs and supplements and vitamins that the patients are taking. Finally, patients will need to provide a list of what drugs they’re allergic to. For the sake of expediency, some patients and caretakers find that it’s easier to have all this information already documented, so it can be passed along when requested. This is especially useful if the patients are unable to communicate.
Patients and their caretakers can also bring personal items. Personal items are generally intended to make the patients more at ease in their surroundings and include comfortable clothing, toiletries, electronics and chargers, reading material and eyeglasses. Items such as cosmetic products or perfumes are usually discouraged.
<p style="clear:both;margin-bottom:20px;"><img src="https://res.cloudinary.com/dqtmwki9i/image/fetch/https://www.project-alpine.com/assets/0174f3fb-10fb-409d-8316-1e52ba20bab7" alt="null" style="max-width:100%;" /></p>
There can be a lot going on when patients are admitted to a hospital. However, the process can be streamlined by bringing or ensuring access to a few key items, according to the Healthcare Consumer Navigator Center: ID card, insurance card, credit/debit card, important health records via patient portal and drug/medication list.
How Do Hospitals Work?
Although hospitals come in various sizes and have various staffing levels, the operational mechanics and best practices remain consistent. First, all hospitals have the same end goal — to achieve the best patient outcomes possible. Hospitals employ several administrative and clinical methodologies to meet this goal.
Medical History and Insurance Information Collection
To appropriately treat and bill a patient, a hospital needs information, which is why triage nurses and other front-line health care professionals serve as the first point of contact. By collecting information about a patient’s medical history (allergies, chronic illnesses, medications, etc.), physicians and nurses have a better idea of how to assess and treat the patient. Additionally, collecting insurance information ensures that the patient is billed correctly once it goes through the insurance carrier.
The Hospital Hierarchical Structure
Patients who are admitted to the hospital enter a facility with a hierarchical structure that’s intended to coordinate care and get them to the right health care providers. The hospital hierarchical structure is as follows:
- Board of directors. The board of directors is responsible for the organization’s direction, its short- and long-term goals, its strategy and its mission statement and vision. The board of directors consists of the CEO, C-suite executives and other high-ranking medical professionals.
- Executive management. Executive management consists of the managers who oversee the hospital. Executive management ensures that the day-to-day operations of the hospital are executed in accordance with the goals and mission statement set forth by the board of directors.
- Department administrators. Department administrators report directly to executive management. They typically oversee a specific department or ward of the hospital, such as pediatrics or the emergency department. Since their work is administrative, they’re also involved in nonclinical departments, such as billing.
- Patient care managers. Patient care managers are the highest-ranking clinical professionals in their departments. The patient care manager is usually the supervising physician or nurse manager on duty. In addition to overseeing and developing a team of clinicians, the patient care manager is the primary resource for handling escalated issues or problems that may arise in their department.
- Clinical health care providers. Clinical health care providers are front-line medical workers who consist of nurses, triage nurses, nurse practitioners and other clinicians. They collect patient information, conduct initial patient assessments and coordinate care when patients are admitted to the hospital.
Improving the Efficiency and Quality of Health Care
There’s always room for improvement in the hospital system. To achieve that, hospitals implement measures to increase health care efficiency and quality. Top methods include the following:
- Focusing on training and education. A surefire way to increase health care workers’ value and experience is by investing in their ongoing training and development. This can be accomplished through peer-to-peer training, workshops, advanced degree programs and on-the-job experience.
- Stressing the importance of proactive measures. The best way to treat patients is to ensure that they don’t become patients in the first place. Primary care providers and family nurse practitioners regularly review the simple ways that their patients can prevent common illnesses. For example, vaccines have an efficacy rate of 50% or above, according to the World Health Organization (WHO).
- Transitioning to digital filing systems. The patient file tells the entire story of the patient’s health care history; however, a hard copy of the file may contain redundancies, can be easily misplaced, is vulnerable to damage and isn’t the easiest to understand. In the digital age, many hospitals are digitizing their patient files to make them more easily accessible, secure and redundancy-free.
- Interdepartmental coordination. Hospitals — especially those located in densely populated areas — are massive facilities with several different departments. When a patient needs to be transferred to another department, time is usually of the essence, which is why interdepartmental coordination is critical to ensuring positive patient outcomes. When different departments know how to collaborate, it greatly decreases the chance of a mistake happening or losing valuable time.
- Reducing patient readmissions. A patient readmission occurs when a patient returns to be admitted to the hospital for the same health care problem. This usually implies that the patient was prematurely discharged or something went awry with the patient’s health following the hospital discharge plan. To reduce hospital readmissions, health care providers should take the necessary steps, such as ensuring that the patient understands the discharge instructions, ensuring that the patient sticks to the medication plan and following up with the patient after discharge.
- Reassessing bed availability. Beds are a finite and valuable resource in the hospital system. During the COVID-19 pandemic, many hospitals discovered that they didn’t have enough beds to accommodate the number of patients seeking health care; this meant that many patients had to be turned away. To help prevent this scenario from reoccurring, many hospitals are applying new models and methods to how to determine bed availability and the number of beds they need to deliver optimal patient care.
- Average length of stay. Patients should neither be prematurely discharged nor confined to a hospital bed longer than necessary; this is why the average length of stay (ALOS) is a critical metric that hospitals track. The ALOS is an indicator of how efficient a hospital is in delivering patient care and serves as a baseline for how long the average patient is expected to be in the hospital’s care. According to data provided by the Organization for Economic Co-operation and Development (OECD), the ALOS for acute care patients was 4 days in 2021; this is on the lower end compared with countries such as Portugal (9.8 days) and Japan (16.4 days).
Billing
Billing is one of the most complex facets of the health care system. The following are some of the core challenges with hospital billing:
- A number of health care providers (over 1,600) each have specific plans and requirements
- Years of government regulations that add to the complexity of hospital billing
- Billing and coding errors that result in incorrect billing or how the insurance carrier processed the health care services
- Patient identifier information that’s incorrect or missing
- Essential documentation that’s missing
- Duplicate billing
- Health care services that the insurance carrier doesn’t cover
Considering the wide array of issues that arise during the billing process, patients need to have a firm grasp on their insurance plans and in-network vs. out-of-network providers, and on how deductibles work. Patients need to also thoroughly review their bills, just in case a service was incorrectly coded, a bill was duplicated or there’s missing or incorrect information.
Fortunately, hospitals and health insurance providers are willing to work together to sort out these types of issues. Patients who notice an error or inconsistency on their bill are encouraged to contact their health care providers immediately.
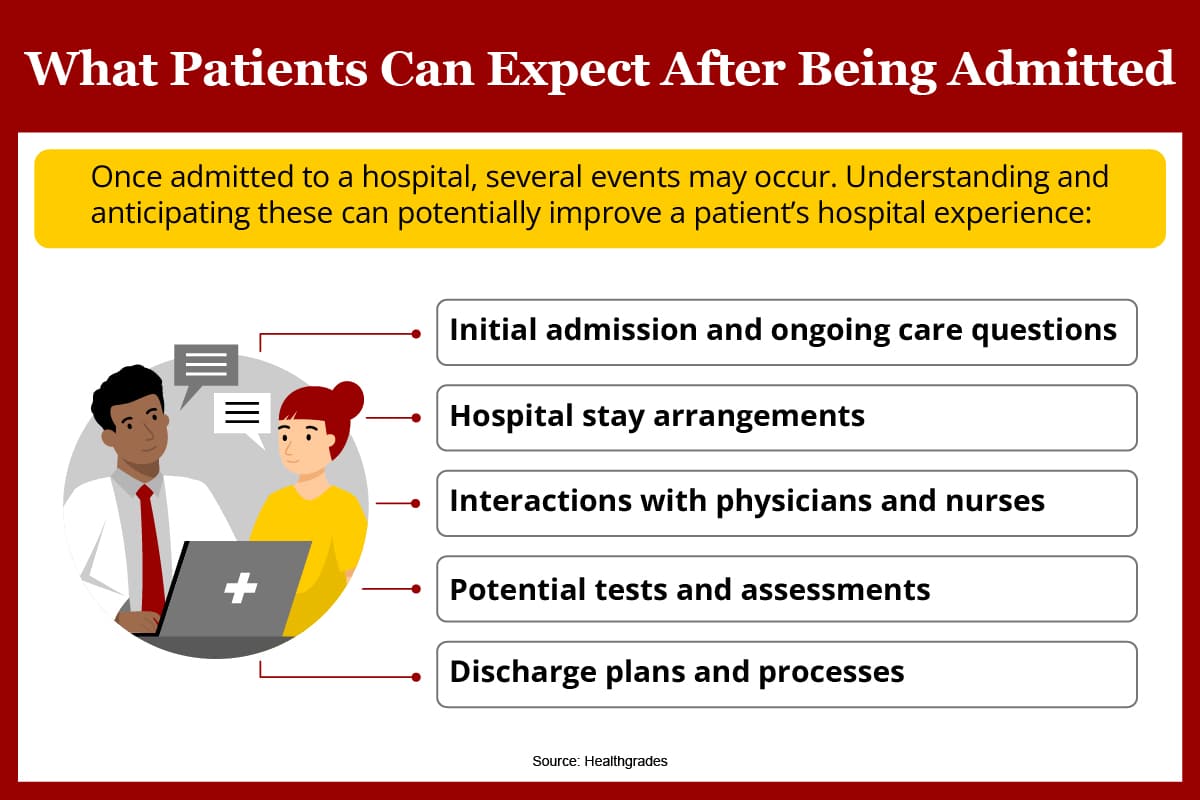
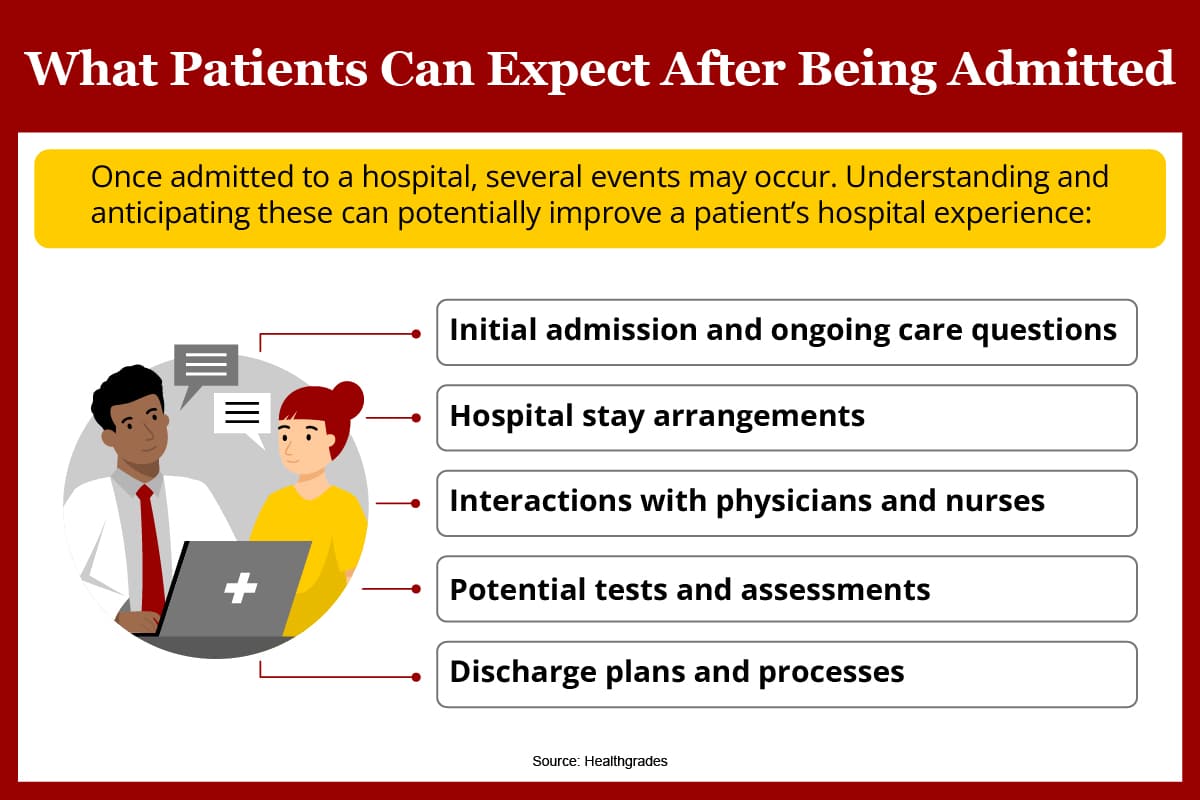
After Being Admitted to the Hospital: What’s Next?
A patient’s individual circumstances help guide which hospital department they’re admitted or transferred to. The following details everything patients should expect once they’ve gone through the initial care and admission questions and are admitted to the hospital:
Basic Amenity Supply
A hospital stay can be a stressful experience for some patients, so providing basic amenities to keep them comfortable is a top priority. The following items are either provided or available for purchase in hospitals:
- Socks
- Pillows
- Blankets
- Music or white noise machines
- Food and beverage
- Women’s health supplies
- Toiletries
- Sanitary items
- Bathrooms
Patients who aren’t emergency admits have more time to figure out what to bring to the hospital. They’re encouraged to pack whatever personal items will keep them comfortable, such as pajamas, electronics and reading material.
Room Sharing
Although many hospitals feature single-patient rooms, patients shouldn’t expect to be assigned to one unless they have an illness that’s a danger to other patients. In all likelihood, patients will be assigned to a shared room with a curtain that separates them from the other patients. This ensures privacy while enabling the hospital to maximize the number of beds they can fit into the space.
Health Care Professional Interaction
Since providing health care services is a group effort, patients should expect several different health care professionals to see them once they’ve been admitted to the hospital. These professionals include nurses, nurse practitioners, student nurses, nursing assistants, physicians and specialists. Patients will also encounter nonclinical workers, such as lab technicians, therapists and dieticians.
Hospital staff members who enter the room will either introduce themselves or relay to the patient what they’re doing there. Additionally, patients always have the right to ask questions or request the attention of a specific health care provider who’s overseeing them.
Testing
Conducting medical tests is critical to patient diagnosis, so it can be determined how best to treat patients. Tests can be as simple as sampling blood or urine, or they can be more advanced, such as taking a CT scan or performing an ultrasound. Regarding tests, medical professionals always make sure to keep the patient informed about the purpose of the test and why they feel it’s necessary.
Dietary Restrictions
Patients’ diets have a direct impact on their bodies. Foods that are high in sodium, saturated fat and sugar may make their current health care conditions worse, which is why many patients are put on a restricted diet once they’ve been admitted to the hospital. Patients with medical conditions such as food allergies, gluten intolerance, digestive issues, Crohn’s disease and diabetes, for example, benefit from a restricted diet. Additionally, patients who’ve recently undergone surgery are put on restrictive diets consisting of clear liquids and foods that are easy on the stomach.
Bedding and Sleep
According to Healthgrades, the average hospital patient sleeps about two hours less than they do at home. Considering that hospitals are unfamiliar settings that are prone to unexpected interruptions and noises, it makes sense that patients have sleep challenges.
The best thing a patient can do in this situation is dull the senses that might cause them to wake up. Patients can use an eye mask to shield them from light and use earplugs or noise-canceling headphones to drown out the noise of the hospital. Patients should also add comfortable blankets and pillows to their list of what to bring to the hospital.
Ongoing Care Questions
Health care providers tend to use medical shorthand (acronyms and so forth) around patients. This can make patients feel excluded or unsure about what’s going on with their treatment. Patients are always allowed to ask about their treatment, whatever stage it’s in. Patients may find that they’re opposed to a certain type of treatment and want to hear about the alternatives. Additionally, patients may find that a certain treatment conflicts with a preexisting medical condition that wasn’t addressed during the admissions process. Patients always have the right to make judgment calls about their care.
Hospital Discharge
A hospital discharge marks the end of a patient’s inpatient care. It means that the patient is to either return home or be transferred to a continuing care facility. The patient always receives discharge paperwork, which consists of the following:
- An explanation of why the patient was admitted to the hospital
- The diagnosis along with any relevant findings
- A detailed summary of the patient’s hospital stay
- The status of the patient’s medical condition at the time of discharge
- A detailed hospital discharge plan
- The signature of the presiding physician
The hospital discharge plan is especially important for patients and their caretakers to be familiar with. Although a discharge signifies that the patient is well enough to leave the hospital, not following the discharge plan may lead to readmission. The main components of the hospital discharge plan consist of the following:
- A detailed breakdown of the patient’s medical issues (including allergies)
- A full listing of medications with detailed instructions on how to take them
- Detailed instructions on wound care (if applicable)
- The dates and times of follow-up appointments along with relevant contact information
- Information on contacts to reach in case of emergency and for general questions
- Dietary restrictions (if applicable)
- Activity-level guidelines
<p style="clear:both;margin-bottom:20px;"><img src="https://res.cloudinary.com/dqtmwki9i/image/fetch/https://www.project-alpine.com/assets/812eae21-179a-4775-ab7a-40c27a0bc9ad" alt="null" style="max-width:100%;" /></p>
Once admitted to a hospital, several events may take place. Understanding and anticipating these can potentially improve a patient’s hospital experience, according to Healthgrades: initial admission and ongoing care questions, hospital stay arrangements, interactions with physicians and nurses, potential tests and assessments and discharge plans and processes.
What Are a Patient’s Rights When Admitted to the Hospital?
Patients who’ve been admitted to the hospital may feel that the situation is out of their control, but they need to know that they have rights that protect them and ensure that they’re treated with decency and respect. Patients are afforded the following rights when receiving medical care:
The Right to Respect
Regardless of personal means, race, ability level, age, gender and other factors, all patients have the right to be treated with respect by their health care providers.
The Right to Obtain Medical Records
The Health Insurance Portability and Accountability Act (HIPAA) of 1996 ensures the legal right of patients to access the entirety of their medical records, including test results and physician notes.
The Right to Medical Record Privacy
HIPAA also ensures that patients can protect the privacy of their medical records, even from health care providers who’ve had access in the past.
The Right to Choose Treatment
Physicians and health care providers will inform patients of what they believe to be the best course of treatment, according to their experience and expert opinion. However, patients who are lucid and of sound mind are free to make a different choice in treatment.
The Right to Informed Consent
The right to informed consent is closely related to the right to choose treatment. What differentiates the two is that informed consent is a structured process of health care providers and staff collecting the necessary information that patients need about their condition, treatment options and other relevant factors so that the patients can make an informed decision. Additionally, physicians are required to confirm that patients fully understand the information that’s been provided to them; this is made official once the patients sign an informed consent document.
The Right to Refuse Treatment
The right to refuse treatment can take many forms. For example, patients may decide that they no longer want to continue taking a certain prescription or get a COVID vaccination. Additionally, they may refuse treatment for religious reasons or due to personal beliefs.
The Right to Decide About End-of-Life Care
When patients are nearing the end of their life, their families can find themselves in difficult situations. Most families believe that a hospital should do everything in its power to keep their loved ones alive; however, the patients might not agree. In this case, the patients need to document their specific wishes well before being admitted to the hospital. The following are some of the key documents and processes relating to the right to end-of-life care.
- Durable power of attorney. A durable power of attorney (DPOA) has the authority to make medical decisions on the patient’s behalf, especially during situations of declining mental function or the patient being incapacitated. When assigning a DPOA, patients need to be sure that they’ll act in accordance with their medical wishes.
- Living will. A living will is an official document that breaks down exactly what treatment the patient is willing to receive in numerous health care scenarios. Essentially, the living will is a guide for physicians that specifies which scenarios the patient wants to refuse medical attention, such as if their heart stops or if prolonging their life would lead to a coma.
Patient Rights Resource Section
For more information about patient rights, check out the following resources:
- American Hospital Association, The Patient Care Partnership: This resource provides a brochure, The Patient Care Partnership, that patients can use to familiarize themselves with their rights and what to expect when admitted to the hospital.
- Cedars-Sinai, Patient Rights: This resource provides a comprehensive breakdown of patient rights relating to service, information, decisions, privacy and protections against surprise medical bills.
- Centers for Disease Control and Prevention, Health Insurance Portability and Accountability Act of 1996 (HIPAA): This resource provides a detailed breakdown of HIPAA and includes covered entities, privacy rules, permitted uses and disclosures and security rules.
- Constitution Annotated, Amdt14.S1.6.4.1 Right to Refuse Medical Treatment: This resource provides official government documentation that breaks down the right to refuse medical treatment with citations from applicable Supreme Court cases.
- MedlinePlus, Do-Not-Resuscitate Order: This resource provides a detailed summary of a DNR that includes its definition, an outline of how the order is created and other key information.
- Verywell Health, “What Are End-of-Life and Advance Directive Documents?”: This resource provides a breakdown of end-of-life and advance directive documents that includes assigning a DPOA, summary and intent of a living will and DNR information.
- Verywell Health, “What Is Informed Consent?”: This resource provides a definition of the term “informed consent” and the medical situations that require it.
Conditions That Require an Ambulance
Individuals should be familiar with the conditions that require ambulance transport. The following situations warrant an ambulance:
Life-Threatening Conditions
Life-threatening conditions or symptoms that indicate a life-threatening situation always warrant ambulance transport. The following are some common examples:
- Exposure or ingestion of a poisonous substance
- Severe pain that comes on suddenly
- Extreme trauma due to a car accident, burns, a large wound or a similar injury
- Bleeding that won’t stop
- Difficulty or inability to breathe
- Blood in vomit
- Extreme injury to the head or spine
When Moving the Person Might Cause Further Harm
Some injuries or illnesses are made worse by forcing the patient to move. A person with a broken leg, for example, shouldn’t try to stand up and walk. Calling an ambulance in these situations ensures that the patient doesn’t further aggravate the condition before being admitted to the hospital.
When Driving or Self-Transport Isn’t Possible
Patients who are unable to drive their own vehicle and can’t secure immediate transport through a caretaker or family member are encouraged to call an ambulance.
When Driving or Self-Transport Could Delay Crucial Treatment
Many emergency situations, such as stroke or extreme loss of blood, require immediate medical attention. If there’s a possibility that self-transport could delay treatment due to safety, traffic or weather, it’s strongly advised to call an ambulance.
When in Doubt, Call 911
Patients who are uncertain about the severity of their health care issue should call 911 to confirm whether their condition requires an ambulance. It’s not uncommon in these situations for dispatch to assist with the process by contacting the nearest ambulance or a local officer to aid with transport.
Why Being Admitted to the Hospital Correctly Matters
Knowing the different ways that patients are admitted to the hospital and what to expect afterward helps provide clarity to the health care system and its processes. When patients know the steps that they’ll go through, such as providing documentation and medical information, it helps streamline the admissions process, so health care professionals can see them more quickly. Keeping the public educated about the types of hospital admissions and what to bring to the hospital promotes better patient outcomes and decreases the likelihood of readmission.
IG Sources:
Healthcare Consumer Navigator Center, How to Plan for and What to Expect During your Hospital Stay
Healthgrades, “9 Things to Expect During a Hospital Stay”
A hospital admission refers to the time that a patient occupies a hospital bed under the care of hospital staff. More than 36.2 million people in the United States were admitted to the hospital in 2019, according to the most recent statistics from Statista. Additionally, the majority of those admitted consisted of seniors 65 years of age or older.